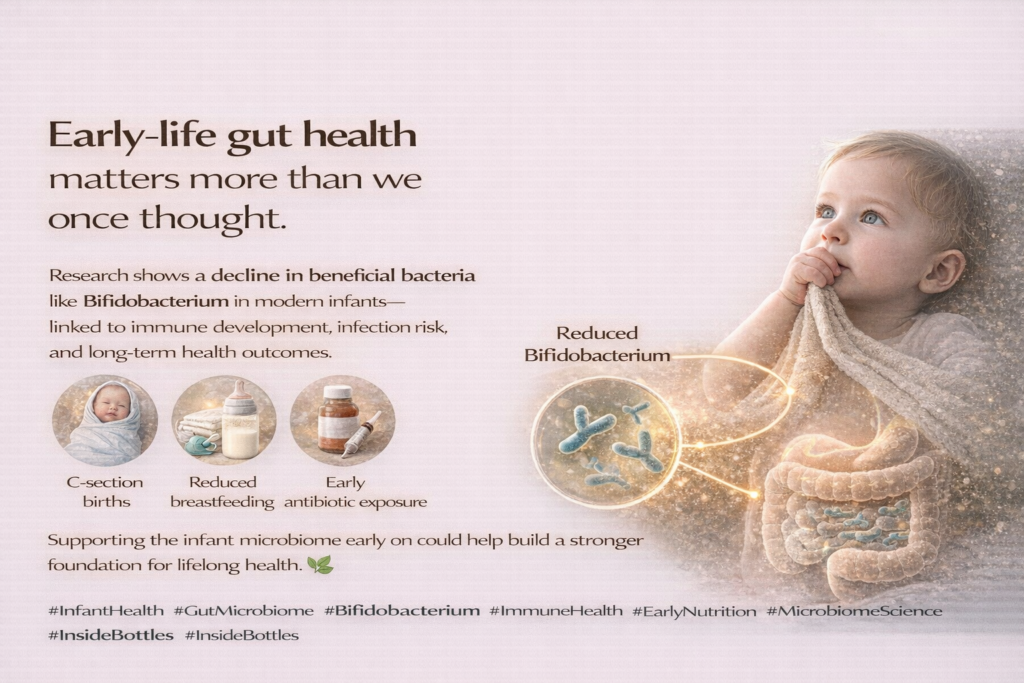
In recent years, research has unveiled alarming changes in the microbial landscape of infants, particularly the significant loss of beneficial bacteria such as Bifidobacterium. This shift impacts not only digestive health but also the development of the immune system, with long-lasting implications on children’s overall health.
Understanding Bifidobacterium
Bifidobacterium is a pivotal genus of probiotics that play an essential role in the gastrointestinal tract, particularly in infants. Known for its unique characteristics, this beneficial bacterium is predominantly found in the intestines of breastfed infants, where it forms a significant part of the gut microbiome. This chapter explores the distinctive qualities of Bifidobacterium, its historical context, and the profound impact it has on establishing a thriving gut environment critical for infants’ immune health.
Historically, Bifidobacterium was first isolated in 1899 by the French microbiologist Albert Calmette. Since then, extensive research has underscored its vital role in gut health. As one of the most abundant bacteria in the intestines of infants, Bifidobacterium aids in the fermentation of dietary fibers, effectively producing short-chain fatty acids that serve as an energy source for colonic cells. These fatty acids also play a crucial part in maintaining gut integrity and reducing inflammation.
The presence of Bifidobacterium in an infant’s gut is particularly significant for several reasons. Firstly, it enhances nutrient absorption by breaking down complex carbohydrates, facilitating the body’s ability to derive energy from these sources. This is especially important during the early stages of development when rapid growth demands efficient nutrient utilization.
Secondly, Bifidobacterium plays an instrumental role in modulating the immune system. It stimulates the production of immunoglobulin A (IgA) and other immunomodulatory factors that contribute to the body’s defenses against pathogens. This early immune programming is vital, as it sets the stage for a well-functioning immune system that can respond effectively to infections.
Furthermore, the benefits of Bifidobacterium transcend mere digestive health. This probiotic genus has been observed to influence the risk of developing allergies and autoimmune diseases later in life. Studies suggest that an adequate presence of Bifidobacterium during infancy is associated with a lower incidence of such conditions, highlighting its long-term significance in shaping health outcomes.
In essence, the loss of Bifidobacterium in modern infants can lead to disruptions in these fundamental processes, risking detrimental health consequences. Understanding the multifaceted role of Bifidobacterium in early life underscores the importance of nurturing a healthy gut microbiome from the very beginning, ensuring infants thrive both in health and development.
The Importance of Gut Microbiota in Infancy
The establishment of the gut microbiota in infancy is a complex, multifaceted process that plays a critical role in a child’s health and immune development. During birth, an infant’s gut is initially sterile, but this changes rapidly as they are exposed to maternal and environmental microbes. Factors such as the mode of delivery significantly influence this colonization; infants born via vaginal delivery are initially colonized by maternal vaginal and gut microbiota, which is known to promote the establishment of beneficial species like Bifidobacterium. Conversely, cesarean section infants often have a microbiome composition that resembles that of skin rather than the gut and are at risk for lower levels of Bifidobacterium.
Breastfeeding further shapes the infant gut microbiome, offering a distinct advantage in the establishment of Bifidobacterium and other essential microbes. Human milk is not just a source of nutrition; it contains specific oligosaccharides that are prebiotic in nature, selectively feeding beneficial bacteria. These oligosaccharides, often termed Human Milk Oligosaccharides (HMOs), facilitate the growth of Bifidobacterium, which in turn produces short-chain fatty acids (SCFAs) essential for gut health and immunity. Notably, Bifidobacterium’s fermentation of these HMOs results in the production of beneficial metabolites that can upregulate the infant’s immune response and regulate inflammation.
The unique bacterial community formed in the gut during infancy is instrumental in teaching the developing immune system to distinguish between harmful pathogens and harmless antigens. This education process is predominantly shaped by the presence of Bifidobacterium, which helps in the production of immune-modulating compounds. The role of this genus is not solely limited to gut health; it extends to the overall development of the infant’s immune system. Disruptions in this initial microbial colonization, particularly a loss of Bifidobacterium, can lead to profound impacts on the immune function and general health outcomes.
Moreover, recent studies have illustrated that the diversity and resilience of the gut microbiome, particularly the presence of Bifidobacterium, can set the trajectory for health not just during infancy but across the lifespan. This emphasizes the importance of supporting the establishment of a healthy gut microbiota from birth through practices such as promoting vaginal deliveries when possible and encouraging breastfeeding to enhance the infant’s microbial ecosystem, thereby fostering optimal immune health and overall development.
Consequences of Bifidobacterium Loss
The loss of Bifidobacterium in modern infancy carries significant implications for children’s immune health, leading to increased susceptibility to a host of disorders. Scientific research has established a strong correlation between diminished levels of this beneficial bacterium and various health complications that can arise in early life and persist into later childhood.
Children with lower Bifidobacterium levels are particularly vulnerable to recurrent infections. This bacterium plays a crucial role in the establishment of a balanced gut microbiota, which is essential for proper immune function. Studies have shown that infants with reduced gut populations of Bifidobacterium tend to experience higher rates of respiratory and gastrointestinal infections, as this microbe is integral in enhancing immune responses and modulating inflammation.
Moreover, the loss of Bifidobacterium has been implicated in the growing prevalence of allergic diseases. Research indicates that a diverse gut microbiota, which includes Bifidobacterium, can help in the development of oral tolerance and prevent the onset of allergies. In contrast, children with a Bifidobacterium deficiency are more likely to develop allergic conditions such as asthma and eczema. A pivotal study observed that infants with a specific lack of this bacterium showed a higher incidence of sensitization to allergens by age two, underscoring the potential long-term consequences on immune health.
Autoimmune disorders also demonstrate a troubling association with Bifidobacterium loss. A reduced presence of this microbe in early life is suggested to disrupt the delicate balance of immune regulation, leading to the inappropriate activation of immune responses. This imbalance could culminate in conditions such as Type 1 diabetes and inflammatory bowel diseases, as the immune system may target the body’s own tissues instead of harmful pathogens.
Furthermore, the impact of Bifidobacterium loss on gut permeability—a phenomenon often referred to as “leaky gut”—can exacerbate these immune-related issues. When Bifidobacterium levels are diminished, gut barrier integrity can weaken, allowing harmful substances to enter the bloodstream and trigger systemic inflammation.
In conclusion, the consequences of Bifidobacterium loss are profound and multifaceted, contributing to increased infection rates, the development of allergies, and potential autoimmune disorders. As our understanding of gut microbiota evolves, it becomes increasingly clear that nurturing Bifidobacterium in infancy is vital for establishing a resilient immune system poised to combat these challenges.
Dietary Interventions for Restoring Microbial Balance
Restoring and maintaining healthy levels of Bifidobacterium in infants is crucial for enhancing their immune health. Several dietary interventions can be employed, focusing on the introduction of probiotic-rich foods, prebiotic sources, and breastfeeding strategies that have been shown to encourage Bifidobacterium growth.
One of the most effective ways to boost Bifidobacterium levels is through adequate breastfeeding. Breast milk provides a unique composition of nutrients and bioactive compounds, including oligosaccharides that serve as prebiotics. These oligosaccharides encourage the growth of beneficial gut bacteria, particularly Bifidobacterium. Experts recommend exclusive breastfeeding for the first six months of life, as this is the prime time for establishing a robust microbiome. Mothers should also aim to sustain breastfeeding alongside complementary foods up to two years or longer, depending on individual circumstances.
After six months, introducing probiotic-rich foods can further support the infant’s gut microbiome. Foods such as yogurt, kefir, and naturally fermented vegetables are excellent sources of live probiotics. When introducing these foods, it’s important to start with small amounts and observe any reactions. Infant-friendly options, especially those specifically designed for younger children, should be prioritized to ensure safety and nutritional adequacy.
In addition to probiotics, prebiotic foods are essential for nurturing the growth of beneficial bacteria. Prebiotics such as inulin and fructooligosaccharides can be found in foods like bananas, onions, garlic, and whole grains. Adding soft, cooked variations of these foods to an infant’s diet can help cultivate a healthy microbial balance.
It is also crucial to promote a diverse diet as infants transition to solid foods. A varied diet introduces different nutrients that can support the establishment of multiple bacterial strains. This diversity is vital as it can lead to a more resilient immune system capable of responding to different pathogens.
Furthermore, avoiding unnecessary antibiotics during infancy is imperative for protecting the existing microbial flora. If antibiotics are necessary, pairing them with probiotics may help restore Bifidobacterium levels more swiftly.
Implementing these dietary strategies early on can create a foundation for lasting health, preventing the detrimental effects associated with diminished Bifidobacterium levels and supporting the infant’s developing immune system. As we strive to understand and improve gut health in children, these interventions provide practical solutions to foster a resilient microbial environment essential for lifelong health.
Future Perspectives on Infant Microbiome Research
As the understanding of the infant microbiome continues to evolve, ongoing research offers promising avenues for enhancing gut health in early life. The mounting evidence supporting the essential role of Bifidobacterium in immune development urges us to explore innovative strategies and interventions to improve microbial health in infants, with a focus on the long-term implications for children’s holistic well-being.
One area of investigation is the potential of targeted probiotic supplementation. Clinical trials are currently examining the efficacy and safety of various Bifidobacterium strains in neonates and infants, particularly those born via cesarean section or those who have been exposed to antibiotics in early life. These studies may yield novel insights into how such interventions can effectively re-establish healthy microbial communities and potentially reverse immune dysregulation.
Moreover, public health initiatives play a crucial role in fostering a better understanding of gut health among parents and healthcare practitioners. By raising awareness about the importance of Bifidobacterium and its impact on the immune system, we can empower families to make informed dietary decisions and adopt practices that promote a healthy start to life. Campaigns aimed at encouraging breastfeeding, promoting the use of human milk banks, and educating about the significance of microbial exposure in early childhood are vital components in this strategy.
Collaboration among researchers, pediatricians, dietitians, and public health officials is essential to translate scientific findings into actionable guidelines. As we investigate the factors contributing to Bifidobacterium loss, it is also critical to examine environmental influences, including chemical exposures, dietary patterns, and urban living conditions, which may alter the microbial landscape. Future interdisciplinary research should focus on creating a comprehensive framework that integrates microbiome data with health outcomes, considering genetic, environmental, and lifestyle factors.
Lastly, raising awareness among parents regarding the lifelong consequences of the infant microbiome is paramount. Providing education on gut health as a pillar of child development can motivate families to adopt practices that foster beneficial microbial diversity. Building a foundation for lifelong health depends on proactive steps taken during this crucial phase of life. Thus, the future of infant microbiome research holds immense potential for reshaping how we understand and support children’s health from birth onward.
Conclusions
The decline of Bifidobacterium in modern infants signals a potential microbial crisis with serious consequences for immune health. Addressing this loss through dietary interventions and promoting beneficial bacteria may help restore balance and improve long-term health outcomes for future generations.
📚 References
-
Henrick, B. M., et al. (2024). Bifidobacterium deficit in U.S. infants and its association with immune development. Communications Biology, 8, Article 123.
https://www.nature.com/articles/s42003-025-08274-7 -
Dominguez-Bello, M. G., et al. (2019). Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proceedings of the National Academy of Sciences, 107(26), 11971–11975.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8211907/ -
Bäckhed, F., et al. (2015). Dynamics and stabilization of the human gut microbiome during the first year of life. Cell Host & Microbe, 17(5), 690–703.
https://pmc.ncbi.nlm.nih.gov/articles/PMC6976680/ -
Laursen, M. F., et al. (2021). Infant gut microbiota development is driven by human milk oligosaccharides and Bifidobacterium. Frontiers in Microbiology, 12, 724449.
https://www.frontiersin.org/articles/10.3389/fmicb.2021.724449/full -
Frese, S. A., et al. (2017). Persistence of human milk oligosaccharide–utilizing Bifidobacterium infantis in breastfed infants. mSphere, 2(1), e00521-16.
https://journals.asm.org/doi/10.1128/msystems.00521-23 -
O’Neill, I. J., et al. (2023). Early-life gut microbiome perturbations precede childhood eczema. mSystems, 8(2), e00521-23.
https://journals.asm.org/doi/10.1128/msystems.00521-23 -
Wang, Y., et al. (2025). Infant-type probiotic supplementation and risk of eczema: A systematic review and meta-analysis. Journal of Nutrition, 155(4), 1023–1034.
https://www.sciencedirect.com/science/article/pii/S002231662500625X -
Henrick, B. M., et al. (2021). Bifidobacteria-mediated immune system imprinting early in life. Cell, 184(15), 3884–3898.
https://pmc.ncbi.nlm.nih.gov/articles/PMC11054607/